

Affiliations
ABSTRACT
An under-studied occurrence, systemic inflammatory polyarticular gout syndrome (SIPGS), represents an acute flare of polyarticular gout with raised inflammatory markers in the absence of any source of infection. It is most commonly precipitated by advanced age, male gender, chronic poorly-treated gout, chronic kidney disease (CKD), and diuretic use. We present a case of a 70-year-old male patient diagnosed with SIPGS along with an unusual cutaneous manifestation, on the background of CKD. He had multiple periarticular tophi with ulceration, discharging chalky-white gritty material. This case is worth-reporting for unexpected systemic inflammatory response activated by polyarticular gout, as well as a unique ulcerative form of cutaneous gout.
Key Words: Tophaceous gout, Polyarthritis, Cutaneous tophi, Inflammation, Ulcer.
INTRODUCTION
Polyarticular gout (PG) is described as gouty arthritis involving multiple joints simultaneously. Long-standing, untreated, or partially-treated PG can culminate into systemic inflammatory syndrome referred to as systemic inflammatory polyarticular gout syndrome (SIPGS), a rarity in the medical literature. The patient typically presents with an acute flare of PG, along with fever and raised inflammatory markers.1 It is vital to identify this entity, as it can mimic sepsis, without any associated infection.2 Both of these conditions have different treatment options. Apart from arthritis, gout can present with a diverse array of cutaneous manifestations, ranging from common periarticular subcutaneous tophi to its atypical ulcerative form, widespread gouty panniculitis, and miliarial gout.3 Herein, we discuss an intriguing scenario of a 70-year male, diagnosed with SIPGS, accompanied by unusual cutaneous manifestation.
CASE REPORT
A 70-year male was admitted via the medical outpatient department with a 2-year history of waxing and waning swelling of multiple joints involving bilateral knee joints, ankles, feet, elbows, and hands.
He had limited mobility and a visible deformity of fingers and toes. He also complained about recurrent cystic swellings in periarticular regions, with drainage of a chalky white material. This material had covered his fingers and toes at the time of presentation. He was previously known to be hypertensive, leading to development of chronic kidney disease (CKD) for the past 4 years, both of which were inadequately treated. His medication included amlodipine 5 mg once daily (poor compliance), non-steroidal anti-inflammatory drugs (NSAIDs), and paracetamol. He belonged to a lower socio-economic class, and there was delay in seeking medical attention.
The patient was vitally stable at presentation, having a pulse of 72 bpm, blood pressure (BP), 140/90 mmHg, SpO2, 98% at room air, and temperature of 98.6°F. On examination, he had multiple, soft to firm, cystic swellings involving bilateral knee joints, and proximal and distal interphalangeal joints of hands and feet bilaterally. A whitish discharge with granules was noticed oozing from cystic swellings, with mild overlying skin redness and warmth (Figure 1). The rest of the clinical examination was unremarkable.
The differential at that point included septic arthritis, rheumatoid arthritis, gouty arthritis, hyper-parathyroid bone disease for joint pathology, and the calcinosis cutis, tophi and rheumatoid nodules for cutaneous lesions.
The investigations revealed raised serum uric acid levels (7.7 mg/dl), elevated erythrocyte sedimentation rate (ESR) at 105 mm/hr, C-reactive protein (CRP), 21.8 mg/l, negative rheumatoid factor (RF) and anti-cyclic citrullinated peptide (CCP), and normal parathyroid hormone levels. X-ray of hands showed subarticular expansile lytic lesions with bone destruction in the head of a proximal phalanx of the thumb, index, and fifth finger along with destruction of joint space and periarticular soft tissue swelling (Figure 2A). X-ray of feet revealed destruction of joint space of the proximal interphalangeal joint of the third finger and distal interphalangeal joint of the second finger (Figure 2B).
Ultrasound examination of the bilateral knee joints confirmed the presence of subcutaneous heterogeneous opacities in the periarticular region, as well as joint effusion. Moreover, gram staining and culture sensitivity of joint aspirate were negative. Aspiration from the knee joint as well as tophi revealed needle-shaped monosodium urate crystals on microscopy (Figure 3), which confirmed gouty arthritis.
 Figure 1: Multiple periarticular cystic swellings with whitish granulated discharge are seen.
Figure 1: Multiple periarticular cystic swellings with whitish granulated discharge are seen.

Figure 2: X-ray of hand (A) and foot (B) showing multiple subarticular expansile lytic lesions.
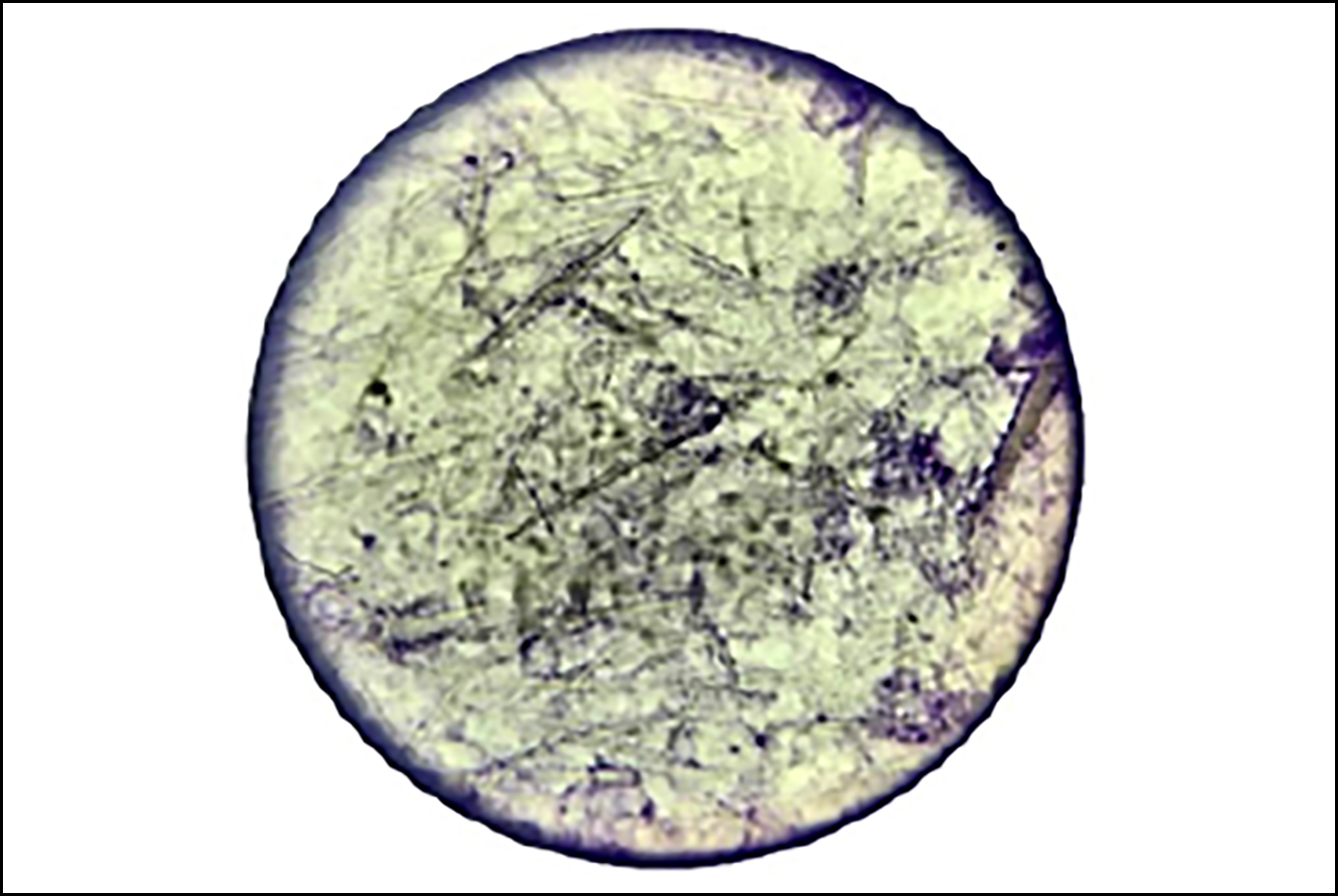 Figure 3. Needle-shaped monosodium urate crystals in knee joint aspirate.
Figure 3. Needle-shaped monosodium urate crystals in knee joint aspirate.
Based on joint aspirate microscopy, raised serum uric acid and inflammatory markers, along with radiological evidence, a diagnosis of SIPGS with ulcerative subcutaneous tophi was made. SIPGS can sometimes mimic sepsis. These can be differentiated from each other on the basis of procalcitonin level, which was negative in this patient.
The patient was started on a short-term course of oral prednisolone, 40 mg/day, in 2 divided doses for 2 weeks followed by tapering over the next 2 weeks. Colchicine was deferred owing to reduced creatinine clearance (14 ml/min). The patient stayed in the ward for 2 weeks, during which his condition improved markedly. The inflammatory markers and cystic swellings settled to much extent. The patient was discharged on febuxostat, 40 mg, daily (renal-adjusted dose), 2 weeks after starting prednisolone. Ultimately, the patient was lost to follow-up.
DISCUSSION
This case captured our interest due to its distinctive cutaneous involvement. Oozing of chalky-white material from the cystic swellings imitated calcinosis cutis and rheumatoid nodules. Upon further investigation, it was revealed that he had an unusual presentation of classical gout. He had an acute flare of polyarticular gout with ongoing systemic inflammation, and multiple ulcerating cutaneous tophi, on a background of CKD. He had raised inflammatory markers, despite no obvious source of infection. It is critical to differentiate SIPGS from sepsis and gout mimics, including septic arthritis, osteomyelitis, rheumatoid arthritis, and hyper-parathyroid bone disease, as their treatment options are entirely different, to avoid unnecessary use of irrelevant medications and potentially delaying definitive treatment of the patient.
A retrospective cohort study conducted in the Czech Republic in 2019 studied 133 gout patients, out of which 17 (12.8%) had polyarticular gout with systemic inflammatory response syndrome (SIRS).4 The activation of the cryopyrin-inflammasome complex by monosodium-urate crystals triggers the release of cytokines, potentially leading to a sterile systemic inflammatory reaction.2 In Pakistan, very limited data is available regarding the prevalence, financial, and health implications of gout, and none about SIPGS. Ashiq et al. reported that gout has a substantially rising burden in Pakistan, but people are suffering in ignorance, and many have joint deformities.5 Indeed, as the disease burden continues to rise, various anomalies and challenges may arise within a healthcare system, as happened in this case. Schafer et al. suggested diagnostic criteria for SIPGS.1 Advanced age, CKD, long-term diuretic therapy, excessive alcohol consumption, delay in initiating urate-lowering therapy, and immunosuppressants have been implicated as risk factors.4,6 In this patient, old age, gender, CKD, and chronic un-treated polyarticular gout probably played a role in the development of SIPGS.
Apart from SIPGS, this patient had another distinctive feature, the expression of chalky-white material from cystic cutaneous sinuses, which were basically periarticular cutaneous tophi. A case with similar cutaneous presentation was reported from India.7 Cutaneous gout can be identified by histopathological evidence of amorphous crystalline material or the presence of negatively birefringent needle-shaped crystals on polarized microscopy.3 Tophus aspirate in this patient demonstrated needle-shaped monosodium urate crystals on microscopy. Lastly, treatment of SIPGS includes NSAIDs, glucocorticoids, or colchicine to induce remission. Once the flare has subsided, then urate-lowering therapy is initiated to keep serum uric acid at sub-saturating levels. These include uricostatic drugs (allopurinol and febuxostat) and uricosuric drugs (mainly probenecid). Pegloticase and IL-1β inhibitors (anakinra and canakinumab) can be used in refractory cases.6,8
In conclusion, this case signifies the diversity of gout symptoms, enabling medical professionals to identify common diseases with atypical presentations. In this case, gout manifested beyond the norm, as SIPGS with unusual skin symptoms. It is crucial to understand that PG attacks can result in a SIRS that mimics infection, especially in people with chronic tophaceous gout. Joint aspirate microscopic examination, ultrasound, and dual energy CT (DECT) are essential for distinction because they enable early initiation of corticosteroids and avoid unnecessary antibiotics or surgery.
PATIENT’S CONSENT:
Informed consent was obtained from the patient.
COMPETING INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
RA, SA: Conception, acquisition and analysis of data, drafting/revising, final approval, accountable for the manuscript.
HN, CUA: Acquisition of the data, analysis, drafting/revising, accountable for the manuscript.
All authors approved the final version of the manuscript to be published.
REFERENCES